This guidance document is part 3 of our series “Protection without pollution: COVID-19 waste-reduction strategies.” These three guides will help health systems, hospitals, and other health care providers set up successful immunization programs that protect the health of people and our planet.
This guidance is for health professionals who are using personal protective equipment (PPE) as they administer vaccinations. It will help vaccine site administrators ensure infection prevention while reducing unnecessary product use and waste. PPE is vital to protect workers and the public, but unnecessary PPE use can result in the needless generation of waste that can also pose risks.
PPE is only one component of a safe community vaccination program. Read CDC's checklist of best practices for vaccination clinics for more information, and follow all applicable regulations for your country. This guidance addresses hand hygiene and PPE use as components of a well-designed vaccination program.
|
Our recommendations
|
Recommendations
Use PPE in accordance with this guidance, and implement hand hygiene when administering SARS-CoV-2 vaccines to maintain infection prevention and reduce unnecessary waste.
Hand hygiene
Hand hygiene is a critical component of any vaccination program, in addition to PPE. Alcohol-based hand rubs are considered best practice in vaccination settings.
Health care professionals should carry out hand hygiene procedures:
- before contact with the patient
- after contact with the patient
- after contact with the patient's environment
- after removal of gloves (when used in special circumstances)
PPE
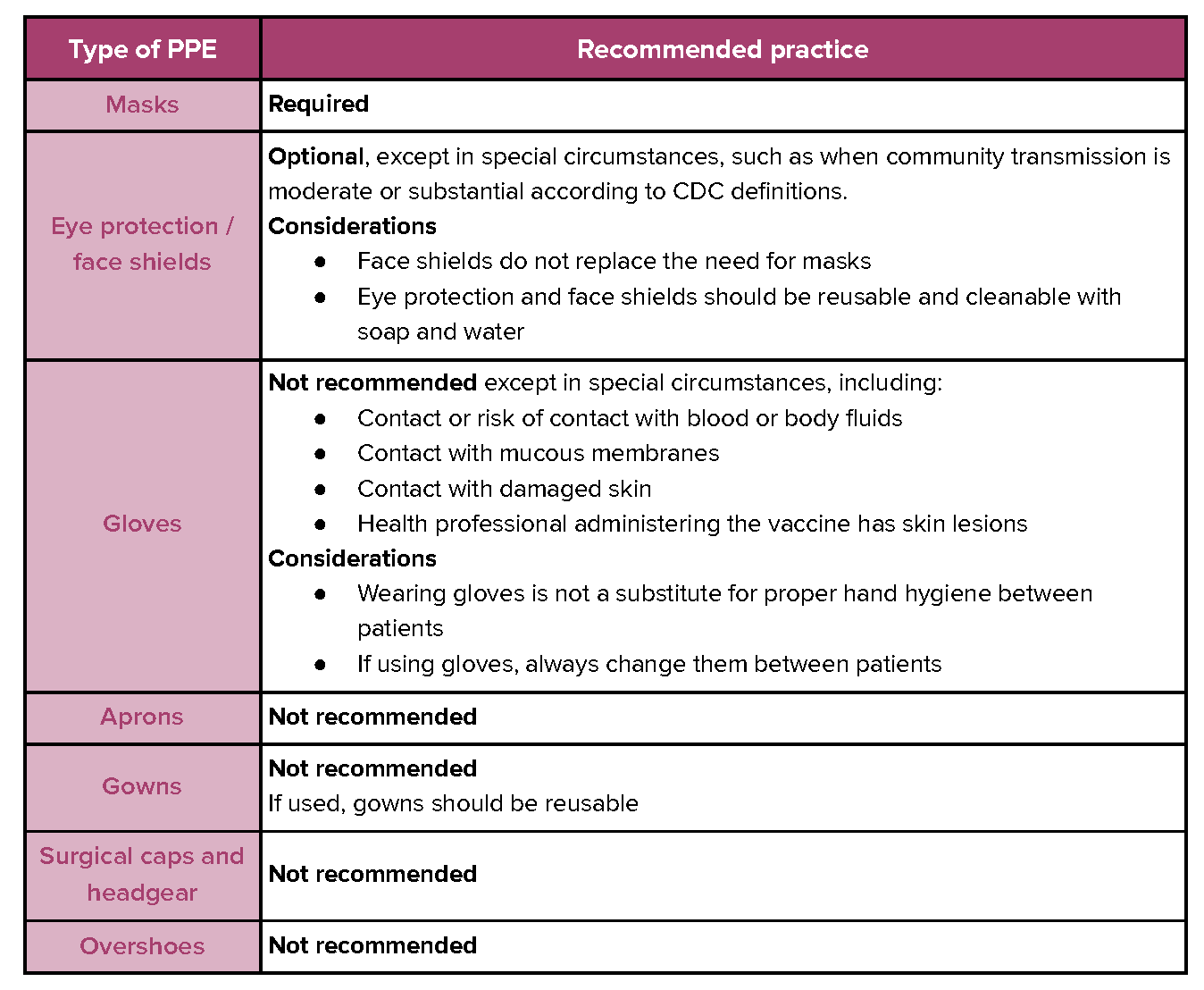
PPE includes eye and face protection, hand protection, body protection, respiratory protection, and hearing protection.
These recommendations are based on and consistent with the guidance of authoritative bodies, including World Health Organization (WHO) U.S.Centers for Disease Control and Prevention (CDC), U.S. Occupational Safety and Health Administration (OSHA), Société Française d’Hygiène Hospitalière (French Society of Hospital Hygiene, SF2H), and Infection Control Africa Network (ICAN).
The recommendations are applicable to all vaccinations sites, unless there are high-risk circumstances requiring additional PPE, including settings where there isn’t prior screening of active cases or there are active cases being treated in the same location as the provision of vaccines. They assume that all vaccine recipients are appropriately masked.
Why develop sustainable PPE practices for immunization programs
There is an urgent need to vaccinate the majority of people on the planet. The scale of this effort will be unprecedented. Additional doses and booster shots will only increase the number of needed vaccinations and resulting waste.
Mass vaccination will generate massive amounts of waste
Industry experts suggest that, as a consequence of the COVID-19 pandemic, global production of medical PPE increased by at least 300% at the peak. Medical mask manufacturing spiked by as much as 1,200% and glove manufacturing spiked by as much as 600%. Shoe covers, aprons, coveralls, and face shields increased 50-100%, and gowns 100-200%. This is expected to continue into 2022. Vaccination programs will significantly increase PPE use. The resulting use of resources in production, distribution, and waste disposal for unnecessary PPE use is significant. Experts estimate around 11 billion doses are required to immunize 70% of the world’s population, assuming two doses per person.
|
Learn more
|
Much of PPE waste can be avoided
Now that we more clearly understand risk factors for the transmission of the virus, some of this PPE use is unnecessary.
Scientific evidence does not support the use of gowns, aprons, surgical caps and headgear, overshoes, and gloves for SARS-CoV-2 vaccination except under special circumstances.
Current PPE used when administering COVID-19 vaccines varies considerably across the vaccine administration sites, according to a survey by a survey by Health Care Without Harm. There are many sites that require the use of single-use gloves, gowns, and other body-covering PPE that have not been demonstrated to be necessary or effective.
Gloves, for example, are often used for vaccination, although they are not necessary except in certain specified circumstances. If 50% of vaccinations were carried out using gloves, an estimated 3-5 billion pairs of gloves would be used.
Gowns are occasionally used for vaccination, although they are not necessary for community vaccination programs. If 10% of vaccinations were carried out using gowns, an estimated hundreds of millions of gowns would be used.
|
Learn more
|
Environmental, health, and human rights concerns
The manufacture and disposal of PPE is generating hazardous chemicals of concern, greenhouse gases (GHG), and waste that further threatens community and worker health.
Environmental pollution is already responsible for diseases and conditions that make exposed populations more vulnerable to SARS-CoV-2, raising ethical concerns.
Increased plastic waste
PPE products are largely made of plastic. Plastic production and disposal pose serious threats to health and the environment, especially when the waste is incinerated.
A 2019 analysis estimated that the production and incineration of all plastic added more than 850 million metric tons of GHG to the atmosphere – equal to the pollution from 189 new 500-megawatt coal-fired power plants.
Half of all plastics ever manufactured have been made in the last 15 years, overwhelming the world’s ability to manage them. Five of the most commonly used polymers use chemicals of concern at every step of manufacturing.
Polyvinyl chloride (PVC), a common material used for gloves, is associated with the use and generation of chemicals of concern at every stage of its life cycle.
Many other plastics are associated with chemicals of concern in production.
Avoiding incineration
Burning hospital waste including PVC gloves as a method of waste disposal can result in the formation of highly toxic chemicals.
The COVID-19 pandemic has led to an “abrupt collapse of waste management chains.” Mismanagement of waste can lead to increased environmental pollution.
Large amounts of waste require collection and recycling, both of which are compromised as a result of labor shortages and efforts to enforce infection control measures.
With fewer options available, traditional waste management practices such as landfills, and incineration are replacing more sustainable measures such as recycling.
Wuhan, China, for example, experienced an increase of more than five times pre-COVID-19 levels of medical waste at the outset of the pandemic.
The incineration or open burning of PPE can release air pollutants that both exacerbate climate change and threaten public health, including impairing lung function.
Climate
According to a new report in the Journal of the Royal Society of Medicine, increased use of PPE in health and social care services in England during the first six months of the pandemic added an additional 1% to the National Health Service’s carbon burden, roughly 27,000 times the average individual in the UK’s daily carbon footprint. The greatest contribution to the total was from gloves, aprons, face shields, and Type IIR surgical masks.
Scenario modeling indicated:
- Eliminating gloves would have reduced the carbon footprint by 45%.
- A combination of in-country manufacturing, reducing glove use, reuse of gowns and face shields, and maximal recycling could have led to a 75% reduction.
- The estimated damage to human health was 239 DALYs (disability-adjusted life years), impact on ecosystems was 0.47 loss of local species per year, and impact on resource depletion was US $12.7m (GBP £9.3m).
Other countries are experiencing an increased carbon burden as well.
Ethical concerns
Recent reports have documented worker exploitation around glove manufacture including forced labor, poor working conditions, and debt bondage. The U.S. Customs and Border Protection agency barred some products from being distributed in the country after finding "reasonable evidence" that the companies were using forced labor. Allegations of abuse in glove production also include passport confiscations, illegal withholding of pay, and restricted freedom of movement.
Governmental guidance
Experts and authoritative bodies from around the globe have provided guidance and best practices for the use of PPE. Our recommendations are based on their guidance.
World Health Organization
“Gloves are not required and, if used, do not replace the need for performing hand hygiene between each vaccine administration and for other indications. Applying alcohol-based hand rubs on gloved hands is strongly discouraged. If gloves are used, they should be removed, hand hygiene performed and a new pair of gloves donned between vaccines.”
European Centre for Disease Prevention and Control
“There is no evidence to date of the protective effect of gloves and gowns for the prevention of COVID-19. The use of gloves and gowns may complicate and prolong the procedure of putting on and removing PPE and may lead to neglecting hand hygiene, and result in contamination of the environment and transmission of other microorganisms in the event that gloves and gowns are not changed after each patient contact. Further research is necessary to clarify the role of gloves and gowns in the prevention of
COVID-19.” – Infection prevention and control and preparedness for COVID-19 in healthcare settings
U.S. Centers for Disease Control and Prevention
“Occupational Safety and Health “Administration (OSHA) regulations do not require gloves to be worn when administering vaccinations, unless persons administering vaccinations have open lesions on their hands or are likely to come into contact with a patient’s body fluids. If worn, gloves should be changed between patients.”
Société Française d’Hygiène Hospitalière SF2H (French Society of Hospital Hygiene)
“The health care professional should “not systematically use non-sterile gloves, but only when the carer doing the vaccination has skin lesions on their hands, in which case they should observe the standard precautions for the use of gloves… Due to the absence of risk of aerosol-generation, wearing an FFP2 mask as well as wearing other protection (gown, apron, eye protection, headgear, overshoes, etc.) are not necessary for the act of vaccination.”
Infection Control Africa Network
- “For screening activities and vaccine administration, only a mask is indicated since there is no splash or body fluid exposure risk during an intramuscular injection.
- Gloves are not indicated for intramuscular or intradermal injections,
- Single-use gloves are indicated if there is any skin breakdown and if used, hand hygiene must still be between each vaccine administration,
- Do not use alcohol-based hand rubs on gloved hands.”
– IPC measures for COVID-19 vaccination roll out
Ministry of Health and Family Welfare, Government of India
This document provides guidance on PPE for COVID-19 vaccination sites, including recommendations for the use of hand hygiene before and after each patient using soap and water or a hand sanitizer that contains 70% alcohol. They recommend wearing a three-layered surgical mask and that hands be sanitized with an alcohol-based sanitizer after vaccinating every patient. They also recommend the availability of hand sanitizer or a handwashing station with soap and water for use by patients and their companions at the entrance of vaccination sites and health facilities, among other recommendations.
