This guidance document is part 2 of our series “Protection without pollution: COVID-19 waste-reduction strategies.” These three guides will help health systems, hospitals, and other health care providers set up successful immunization programs that protect the health of people and our planet.
The world is undertaking the largest immunization campaign in history to fight COVID-19. Billions will be vaccinated in the coming years, which is generating an unprecedented amount of waste. If we plan ahead, we can minimize the impact and waste while ensuring universal immunization.
|
Our recommendations
|
Why develop an immunization waste management program
Over 153 million cases of COVID-19 have been confirmed worldwide, including 3.2 million deaths. Global efforts to respond to the pandemic are continuing, with laboratory, treatment, and immunization capacity expanding. By May 2021, 14 vaccines had been approved in at least one country, and over 100 were in preparation. Globally, over 1billion vaccine doses have been administered. This includes almost 50 million shipped to low-income countries by the World Health Organization (WHO) COVAX facility, part of an effort to provide at least 2 billion doses during 2021. Over 17 million test kits and 200 million separate items of personal protective equipment have been supplied to date.
|
Plan to prevent pollution Much of the waste from vaccination can be avoided, minimized, or recycled. Health care professionals and governments can use strategies like careful planning, rethinking delivery and implementation, and prioritizing reuse and recycling to eliminate as much waste as possible and work toward the goal of a zero-waste immunization program. |
This unprecedented immunization campaign comes at a time when only 39% of countries have national programs on infection prevention and control, water sanitation, and health care waste management.
The huge need for masks, gloves, and other personal protective equipment, millions of COVID-19 tests and lifesaving hospital treatment for victims of the disease has led to an increase in health care waste. In the early stages of the pandemic, some locations faced a 5-6 fold increase in healthcare waste, partly due to classifying all waste as infectious as a precaution. The global market in face masks was projected to increase more than 200-fold in 2020. The increase in PPE use significantly impacts these products’ climate footprint. Improper PPE disposal by hospitals and households is adding to the burden of plastic pollution.
COVID-19 vaccine waste and its hazards
The vaccination process can generate many types of waste, which can worsen health, climate, and environmental pollution.
Agencies who manage vaccination campaigns often fail to collect and return immunization products to the original distribution centers for reuse, recycling, and disposal. This process is also known as “reverse logistics.” It is vital for a successful immunization waste management program.
The burden of waste management falls on the people managing the vaccination centers, which may be a remote location without the expertise or resources for waste management. Consequently, much of the waste is unsafely burned or dumped.
Cold chain and transportation
The cold chain and transportation of vaccines can generate packaging waste, dry ice, emissions of refrigerants, and ultimately electrical and electronic waste in the decommissioned fridges, freezers, and tracking devices.
The mRNA vaccines require the most careful storage, including freezers for the Moderna vaccine and ultra-cold freezers for the Pfizer vaccine. The vaccines are transported in special containers using dry ice which can maintain minus 70 C / 94 F for 10 days unopened or thirty days if the dry ice is topped up. Thereafter, they can be kept at 2-8 C / 35.6-46.4 F for five days. Some shipping containers are mostly cardboard and designed to be returned to the manufacturer, a practice that should be expanded to reduce shipping and packaging waste.
Dry ice is frozen carbon dioxide gas, which can cause burns, so handlers should wear PPE including gloves and goggles to prevent it from coming into contact with the skin. It will turn back into gas at temperatures over minus 78 C / 108.4 F. If this happens in a confined space, it can cause suffocation.
Disinfectant wipes
Disinfectant wipes are made from a wide variety of natural and synthetic materials, saturated with a disinfectant such as isopropyl alcohol or chlorhexidine. They are often individually wrapped in packages of paper, plastic, and foil, which are not recyclable. Swabbing the injection site is not medically essential, so time, money, and waste can be saved by minimizing or eliminating the practice. When they are used, wipes should be biodegradable, minimally packaged, and contain alcohol as the disinfectant. The flushing of wipes can cause sewage problems, so it is best to avoid flushing them.
|
What makes an injection ‘safe’? “Does not harm the recipient, does not expose the provider to any avoidable risks, and does not result in waste that is dangerous for the community.” – World Health Organization |
Syringes and needles
Single-use syringes are essential. If syringes are not disposed of properly, waste handlers or members of the public can be injured.
Vaccine waste and empty vaccine vials
It is essential to store and transport vaccines, especially the mRNA vaccines, at the correct temperature to avoid spoilage and waste. Unused vaccines are not hazardous and do not need any special treatment. Vials should be returned for reuse or recycled wherever possible.
In the future, delivering COVID-19 and other vaccines in pre-filled syringes could eliminate this type of waste. However, pre-filled syringes would probably take up more space than the multi-dose vials in use, putting extra pressure on cold chains.
Contaminated and non-contaminated PPE
All used PPE should be treated as infectious waste. Vaccinators should avoid the use of unnecessary PPE. Gloves are generally not necessary.
|
Learn more
|
Waste management options
Fortunately, the same waste management practices which protect against infection and other hazards, are effective at treating and preventing waste from COVID-19 patients.
Waste minimization
Established waste segregation practices should be reinforced, but there is no need to classify more waste than normal as infectious. PPE is vital to protect workers, but excessive PPE increases waste as well as wasting scarce resources. It can also make it harder for health professionals to do their job. For example, staff providing vaccinations do not generally need gloves and using them can reduce dexterity.
Wherever possible, waste should be recycled, reducing the amount that needs disposal.
|
Learn more
|
Avoiding incineration
There is no technical reason why vaccination waste needs to be incinerated. As health systems expand waste management capacity in the face of the pandemic, it is important to avoid using or investing in technologies that cause pollution (also known as “regrettable investments”).
Avoiding toxic substances
Although some insulating COVID-19 vaccine packaging is cardboard, expanded polystyrene is commonly used. Polystyrene is rarely recyclable and the main feedstock, styrene, is harmful and a potential reproductive toxin. Plastics with environmentally harmful life cycles (e.g., PVC) should be designed out of all components of the vaccine delivery chain, from packaging to gloves and wiring in refrigeration units.
Toxic disinfectants and excessive use of disinfection products should be avoided.
Refrigeration should not use hydrofluorocarbons (HFCs), as many are potent greenhouse gases.
Worker protection
Most countries have prioritized health workers for coronavirus vaccination. People who handle waste should be given priority access to vaccinations for the coronavirus and other vaccine-preventable diseases; and, as needed, offered post-exposure prophylaxis.
Everyone involved in the COVID-19 vaccination process should be provided with PPE, including waste management workers. Auto-disable syringes, which can only be used once, are recommended by WHO and UNICEF. This avoids illicit and dangerous reuse of syringes.
‘The polluter pays’
Manufacturers should contribute to the costs of waste disposal through extended producer responsibility mechanisms. This could include funding for product takeback and environmentally friendly treatment, recycling, and disposal.
How to implement an immunization waste management program
Successful implementation of a vaccination waste management program will involve careful planning at central and local levels, a financing and management structure, clear assignment of responsibilities, adequate briefing and training of staff, daily monitoring and immediate corrective actions wherever necessary, and final evaluation and recommendations for future actions.
Step 1: Planning
- Review relevant national legislation, or, if there is no national legislation, international guidance on health care waste management disposal, worker and environmental protection
- Estimate how much waste each vaccination site will generate
- Map suitable current waste treatment and disposal facilities
- Cluster vaccination sites around selected waste disposal facilities
- Organize the collection and transportation of the waste to the disposal sites identified
- Formulate a detailed plan for the waste collection, transport, and disposal
- Obtain financing and other resources for the implementation of the plan
Step 2: Waste avoidance, minimization, and recycling
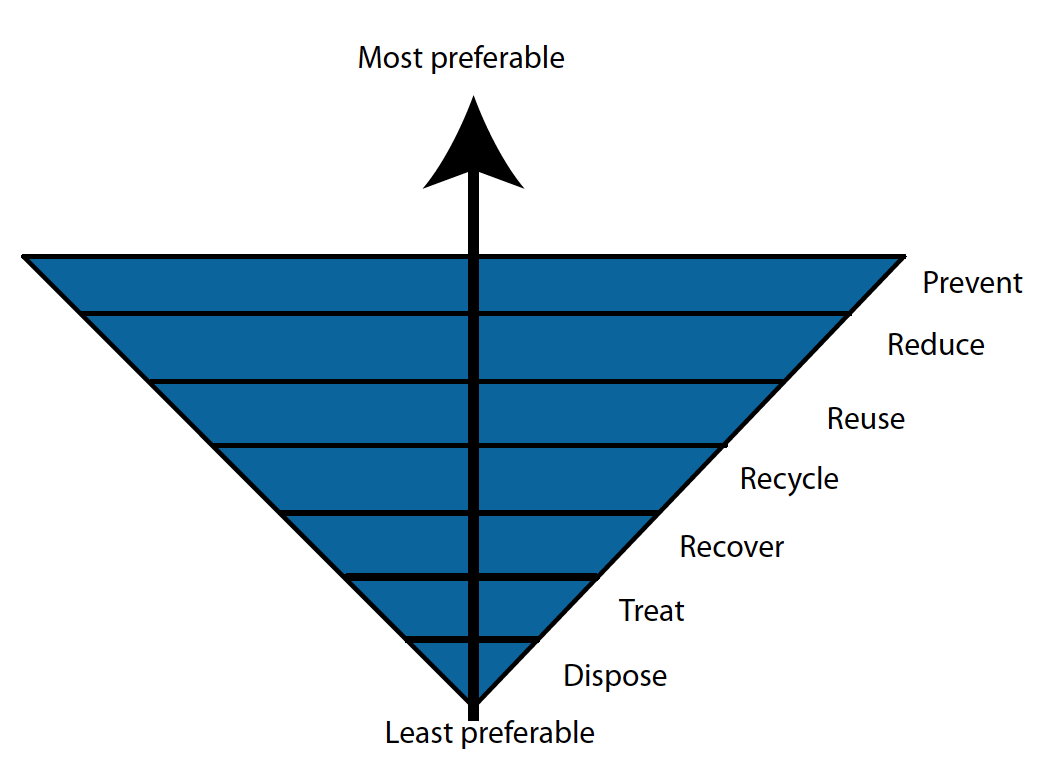
The first priority for waste is waste avoidance, including the procurement of reusable products, and products that generate the least amounts of waste, and the least toxic waste. Potential for recycling, which reduces the amount of waste needing disposal, should also be included in procurement criteria.
Alcohol is the disinfectant of choice for use against SARS-CoV-2, in products like disinfectant wipes and hand sanitizer. Soap and water should also be available for hand hygiene.
The choice of syringes can help reduce vaccine and vial waste. Pfizer vaccines are supplied in five-dose vials, and by using low dead-space syringes, six doses are possible. Oral vaccines, which supplement injectables or eliminate the needle and syringe altogether, are at an early stage of development, and it is not certain if or when they may become available.
Step 3: Waste treatment and disposal
Dry ice must be removed from shipping containers before they are stored in cold rooms or freezer rooms. It should be allowed to sublimate back into gas in a well-ventilated area at room temperature and not left in an unsecured area, disposed of via drains or flush toilets, or in the trash.
Waste generated at vaccination centers should be segregated so that each type of waste is dealt with in the most economical and environmentally friendly manner. There is no need to double-bag waste or spray it with disinfectant. General waste, including alcohol swabs, should be disposed of in the normal manner.
Packaging and vials should be returned for reuse or recycling, monitoring security considerations. The scarcity of vaccines means that packaging and vials are in demand by counterfeiters and should be tracked to their final destination. If they are not to be reused, they should be shredded or crushed to prevent copying.
PPE and used syringes should be classified as infectious waste and disinfected via non-incineration methods. The most widely used options are steam-based, particularly microwave and autoclaves. Autoclaves are familiar technologies in health care, and models designed specifically for waste are available in a range of sizes and designs.
Syringes should have the needles removed with needle cutters, which reduce the volume of waste without increasing the risk of injury to vaccinators and make the waste safer to handle and treat. (Some countries, including the United States, do not permit needle cutters except when no other option is available.) They should be collected in puncture-proof sharps containers that are ideally reusable. If facilities are available for processing, syringe plastic can be disinfected and recycled.
|
Learn more
|
Case studies

In Madagascar, autoclaving was used to disinfect syringes before disposal. (UNDP)
Disposing almost 20 million syringes without incineration (The Philippines, 2004)
In 2004, Health Care Without Harm and the Philippine Ministry of Health collaborated during the Philippines Measles Eradication Campaign to demonstrate how it was possible to dispose of almost 20 million syringes without the need for incineration. Centralized disinfection via autoclaves and microwaves proved among the most economical methods. The participants identified needle cutters, reusable sharps containers, and recycling as important strategies for the future.
The vaccination campaign targeted 18 million children and generated almost 20 million syringes in sharps boxes, representing 130 metric tonnes (143 tons) of sharps waste and 70 metric tonnes (77 tons) of non-hazardous waste including empty vaccine vials and ampoules, syringe wrappers, empty vitamin capsules, cotton swabs, syringe caps, and packaging. Syringe waste was brought to central storage areas and then disinfected via microwave or autoclave. Where those technologies were not available, sharps waste was encased in a concrete septic vault or buried in a waste pit. Centralized microwaving and autoclaving had equivalent costs and were cheaper than either concrete vaults and cement floored burial pits. Burial in a clay-bottomed pit was the cheapest and the entire project was carried out without the need for incineration of any waste.
|
Learn more
|
Recycling immunization materials (Nepal, 2014)
Some of these concepts were tested in 2014 in Nepal, and it was found possible to recycle not only syringe plastic, but cardboard and plastic packaging, vials, and aluminum caps. Autoclaving and recycling were found to be more economical and had a lower carbon footprint than incineration or open burning.
Autoclaving during a measles outbreak (Madagascar, 2018-2019)
During a measles outbreak in Madagascar, the University Hospital Ravoahangy Andrianavalona (CHUJRA) Ampefiloha assisted in the autoclaving of vaccination waste. Autoclaves used for the hospital’s health care waste were deployed to disinfect syringes in sharps boxes from vaccination sites that would otherwise have been open-burned. This was a project funded by Global Environment Facility (GEF) and facilitated by UNDP, WHO, and Health Care Without Harm.
