2015 Sustainable Operations Survey

by Beth Burmahl, Suzanna Hoppszallern Senior Editor, Jamie Morgan
Hospitals make fruitful progress toward sustainability as some take great strides and others stick to baby steps
 |
When it comes to environmental sustainability, hospitals across the United States are making considerable strides in lopping off what industry experts call the low-hanging fruit — the less costly and labor-intensive measures that often show significant energy and cash savings.
But reaching the fruit nestled higher up in the tree — purchasing bigger-ticket items, securing adequate staffing and developing comprehensive sustainability programs that address the issue from every angle — may take significantly more time. “The first step for hospitals is usually reducing energy consumption,” says Robin Guenther, FAIA, LEED Fellow, principal of Perkins+Will. “Once they have implemented the basic components of energy conservation — the low-hanging fruit — then they are in a position to move to the next level.”
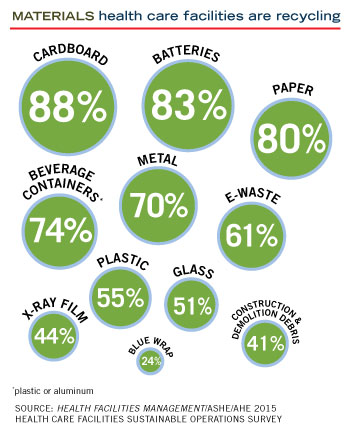
So, while most hospitals haven’t embraced measures like using rainwater for landscape irrigation or purchasing off-site renewable energy, they continue to make progress in initiatives such as installing light-emitting diode (LED) exit signs, commissioning or retrocommissioning of buildings, upgrading building control and automation systems and recycling everything from cardboard to electronic waste.
That’s one of the takeaways from the 2015 Health Facilities Management (HFM) Sustainable Operations Survey conducted with the American Society for Healthcare Engineering (ASHE) and the Association for the Healthcare Environment (AHE), the first HFMsurvey on green initiatives since 2013. During that time, hospitals have continued to make slow but steady gains in embracing sustainability issues, showing only modest increases or decreases in most categories.
As with two years ago, roughly 70 percent of hospitals are measuring energy savings, but the vast majority still are not using performance metrics to track their energy budgets.
While the survey shows that hospitals are committed to the goals behind sustainability — 80 percent named improved operational efficiency as the top factor influencing green measures — progress continues to be hindered by such factors as the economy, staffing concerns, the fight for capital dollars and CEO support for green initiatives.
While facilities are at various stages of embracing sustainability, about half of those surveyed have yet to create a formal sustainability program or even put together a committee to get things moving. And close to 60 percent say they have no C-suite representative on their team — something that would go a long way toward creating awareness and gaining buy-in for environmentally focused projects.
About This Survey |
|
Health Facilities Management, the American Society for Healthcare Engineering and the Association for the Healthcare Environment surveyed a random sample of 4,158 hospital executives to learn about trends in sustainable hospital operations. The response rate was 6.6 percent, or 276 completed surveys. |
“I think sustainability is gaining ground with many CEOs, although some may think it is a costly endeavor. Nothing could be further from the truth,” says ASHE President-elect Terry M. Scott, CHFM, CHSP, SASHE, director of engineering/construction services, Memorial Hermann Northwest and Memorial Hermann Southwest hospitals in Houston. “An aggressive energy-reduction program can reduce a facility’s energy expense by $2 per sq. ft. That translates into millions of dollars saved annually.”
For example, at Memorial Hermann, Scott says eight of their 10 eligible hospitals have earned the Energy Star label, saving more than $76 million in five years. “Numbers like that get the attention and support of the CEO and C-suite,” he says.
Overcoming roadblocks
The good news is that it doesn’t take a lot of money to start saving energy, says Clark Reed, who heads the Environmental Protection Agency’s (EPA’s) health care program for Energy Star. “Retrocommissioning, for example, is one way many hospitals begin to cut energy because it’s a cost-effective method to quickly demonstrate cost effectiveness to senior leadership.”
The survey showed that 42 percent of respondents have implemented or plan to use commissioning or retrocommissioning — an audit to review building performance of energy systems — a low-cost measure that can yield big savings. One survey respondent noted: “As a result of retrocommissioning a number of buildings, we have saved approximately $600,000 in steam and over $250,000 in electricity.”
But while cost savings can be a huge incentive, funding also topped the list of roadblocks to implementing environmental projects. Sixty-one percent named competing investments/spending priorities as the top challenge/barrier to realizing environmentally sustainable measures, followed by employee time limits (52 percent) and lack of adequate staff (50 percent).
Asked to rate the factors influencing their pursuit of sustainability, 80 percent named improved operational efficiency followed by long-term cost benefits (76 percent), patient care quality initiative (74 percent) and consistency with the hospital mission (68 percent).
That type of disconnect may be preventing hospitals from fully realizing their sustainability goals, says Laura Faye, owner of Blue Environmental Performance Consulting, San Francisco.
 “When you compare the influences and the barriers, they aren’t aligned,” says Faye. “These goals would be in line with any hospital or CEO’s mission, but the survey shows that hospitals aren’t providing the funding for their staff to meet these sustainability goals.”
“When you compare the influences and the barriers, they aren’t aligned,” says Faye. “These goals would be in line with any hospital or CEO’s mission, but the survey shows that hospitals aren’t providing the funding for their staff to meet these sustainability goals.”
Although more hospitals are designating one position to be responsible for environmental sustainability — a strategy that is key to aiding green efforts — the numbers are only inching up. In 2015, the survey showed that 29 percent had designated a sustainability manager, up from 23 percent in 2013.
“For what it costs to pay one full-time person, the facility could save millions of dollars,” says Scott. “That person would pay for himself in a year easily.”
As the sustainability coordinator at Gundersen Health System, La Crosse, Wis., Tom Thompson is just one member of a facilities leadership team that includes a comprehensive waste manager, an environmental compliance manager in charge of pharmaceutical waste, and a facilities manager whose engineering skills tie in perfectly with his role as the manager of energy conservation.
All team members are focused on the same goal, Thompson says. “We all have it in the front of our minds that we are here to do the right thing for the environment and the health of our community, but we also strive to be economically responsible as well. We have to fight for budget dollars — they’re not just handed to us.”
The team is constantly evaluating and re-evaluating current programs while keeping its collective eyes open for the next sustainability opportunity. Their mantra — “this is a process, not a project” — keeps the group focused.
“But we have to prove our worth,” Thompson says. “We have very good metrics on the cost-saving opportunities that we generate by having our positions strategically placed within the system.”
On pharmaceutical/hazardous waste alone, Gundersen has cut costs by more than 70 percent since establishing a baseline for measurement in 2010 — adding up to more than $100,000 in savings each year.
Energy metrics
Although 69 percent are measuring energy consumption, many hospitals — in fact the majority of those surveyed — still are not tracking performance metrics. Only 37 percent include performance metrics, such as the EPA Energy Star rating, total waste generation or a recycling rate, in their senior management dashboards — roughly no change since 2013.
In terms of energy-performance monitoring tools, the two most frequently used are energy audits (44 percent; no change from the 2013 survey), while 45 percent set and monitor energy budget and performance targets, up from 39 percent in 2013.
“It’s interesting that a large number are tracking, but fewer are setting energy goals and targets,” says Janet Howard, director of member engagement, Healthier Hospitals program, Practice Greenhealth. “Collecting data without targets is a lost opportunity for savings.”
“Tracking is absolutely critical,” says Faye. “If you’re tracking your energy performance and spending, there is an opportunity to reduce both. You can’t manage what you don’t know you’ve got.”
Another 34 percent track energy performance in EPA’s Energy Star Portfolio Manager or use the Energy Star Target Finder for new design performance targets; 16 percent participate in ASHE’s Energy to Care Program, and Scott says the ASHE program is quickly gaining ground. “There are now over 1,315 buildings benchmarked on ASHE’s Energy to Care website, which represents 535 hospitals,” he says. “My goal as president will be to increase those numbers dramatically.”
Some hospitals are using in-house tracking initiatives. One hospital surveyed has assembled a team to review, trend and critique energy usage on a monthly basis via meter readings, utility bills and work order data broken down into usage per day, comparing numbers to the same month for the previous three to five years. “This process identifies outlier energy usage per meter where a more thorough investigation occurs to find the ‘energy hog.’ These are low-cost but require significant labor resources.”
Other facilities surveyed in 2015 are doing piecemeal upgrades when resources allow.
“We do not track energy use to verify energy or resource savings; however, we spend a few extra dollars when we replace items either as a maintenance task or as part of a larger renovation project,” one survey respondent said, “for example, replacing a toilet with a low-flow fixture and valve when a toilet needs to be replaced.”
Waste watch
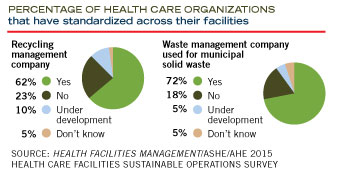
Although hospitals produce more than 5.9 million tons of waste annually, facilities still have work to do in terms of waste stream reduction. While 97 percent have a regulated medical waste program and 93 percent have a pharmaceutical waste program implemented or in progress, just 61 percent reported having an ongoing process for tracking waste volume and cost for all waste streams, an increase from 46 percent in the 2013 survey.
The tracking numbers are surprising to 2015 AHE board president Greg May, CHESP — especially considering the number of regulations governing waste and the dialogue surrounding waste reduction. “The numbers are puzzling, since every facility I’ve seen has some kind of waste-tracking mechanism in place, and some have instituted aggressive plans for waste reduction,” May says.
 For example, the University of California has a program to reach zero waste by 2020 for all of its hospitals, Scott says. Individual hospitals are also making big strides. In theHFM survey, one facility reported cutting the amount of regulated medical waste generated through improved segregation in the patient rooms (fewer red bags), and also selected one vendor for regulated medical waste for an estimated savings of more than $1 million in 2014.
For example, the University of California has a program to reach zero waste by 2020 for all of its hospitals, Scott says. Individual hospitals are also making big strides. In theHFM survey, one facility reported cutting the amount of regulated medical waste generated through improved segregation in the patient rooms (fewer red bags), and also selected one vendor for regulated medical waste for an estimated savings of more than $1 million in 2014.
Additionally, recycling is a high point among respondents, with standard items like cardboard, paper and batteries scoring the highest (88, 80 and 83 percent, respectively) in the survey. And some initiatives are just getting off the ground. For example, one facility instituted an organic recycling program to separate organic from regular waste, diverting more than 70 tons of waste that became “fuel” for the city’s yard waste program.
While many are tracking material and waste generation, Practice Greenhealth data analysis demonstrates that the data integrity could be improved, Howard says. “Multiple materials are removed by multiple vendors. Coordinating and capturing data from a variety of sources is key. Practice Greenhealth considers composting as a component of the recycling stream but does not count single-use device reprocessing toward recycling rates. Lastly, using generic conversion factors can throw generation rates way off — weigh a sampling and create your facility’s own conversion rate.”
That may explain why nearly half of survey respondents answered “Don’t know” when asked for the percentage by which they have reduced waste stream volume and expenditures through sustainability measures in the past year.
Tapping water
While water is the next big thing in sustainability, most hospitals are tackling the least expensive upgrades before going further. Participation also may hinge on what part of the country a facility is located.
Most upgrades center on such things as installing low-flow control fixtures on faucets (49 percent), and low-flow fixtures on toilets/urinals (52 percent) and using a closed system for cooling to reduce process water (50 percent), the survey shows. “Those things make a lot of sense to implement,” Faye says. “They pay for themselves.”
Facilities also can take advantage of financial incentives for installing water- efficient equipment. As another incentive, LEED offers water-efficiency credits.
Hospitals in drier regions of the United States will be relying on water audits and turning to initiatives such as drought-tolerant landscaping or condensate recovery systems to deal with the water shortage, says Guenther. “The California drought is going to bring forward some people doing pretty interesting sustainability work in that part of the country,” she says.
Faye says she would like to see more hospitals creating water management plans. “Many hospitals now facing a drought are scrambling because they don’t have a plan in place,” Faye says.
Cleaning up
Green cleaning continues to gain momentum as hospitals work to create infection-free environments for their patients and staff.
The top sustainable cleaning initiatives on the 2015 survey also scored the highest in 2013 — 89 percent use microfiber mops to reduce water and chemical use, and 78 percent use cleaning equipment that doesn’t negatively affect indoor air quality.
But in terms of metrics, May says many facilities aren’t yet on that track. “Almost every environmental services director has some kind of green cleaning program — water, chemical-free stripping of floors, low-odor chemical — but I don’t know if many hospitals have a formal metric,” says May. “Someone is likely monitoring progress, but not in a formal way.”
Asked whether they track and report savings from sustainable cleaning practices, a resounding 79 percent responded “No.”
Resources abound
Of all the data that came from the 2015 survey, sustainability experts say they are most puzzled by the low number of participants involved in the many programs offering free resources for reducing their environmental footprints.
“I have attended meetings with large numbers of facilities managers, and I have asked them if they are benchmarked on the Energy Star site, and only a few hands are ever raised,” Scott says.
Nevertheless, there is no shortage of resources hospitals can access. Among them, ASHE’s Energy to Care Program provides a free benchmarking and dashboard tool to measure and track a facility’s energy use. Developed by ASHE, AHE and the Association for Healthcare Resource & Materials Management, the Sustainability Roadmap for Hospitals (www.sustainabilityroadmap.org) shows facilities how to implement real-world sustainability projects, enhance existing efforts and share their environmental successes with others.
“In addition, the Hospitals in Pursuit of Excellence guide on sustainability includes a matrix of these measures and their various investment levels,” says Patrick Andrus, ASHE’s deputy executive director of operations.
ASHE also is in the process of creating a task force to develop a list of individuals who will provide free benchmarking assistance and a roster of companies that will provide free energy audits to hospitals, according to Scott. The resources are slated to be available in January 2016.
Another growing trend is staging energy challenges where hospitals strive to save the most energy in one year. The EPA and ASHE have sponsored such energy challenges nationwide for a number of years with great success across the board.
“Hopefully, these types of projects will lay the groundwork for new green initiatives down the road,” Guenther says.
“In general, you’re only going to see large numbers of hospitals implementing new programs if a small group of innovative hospitals have done it first,” Guenther adds. “People want to see what they’re talking about in action.”
Beth Burmahl is a freelance writer based in Oak Park, Ill., who specializes in health care topics;Suzanna Hoppszallern is senior editor of data and research for Health Facilities Management’s sister publication, Hospitals & Health Networks; and Jamie Morgan is associate editor for Health Facilities Management.
Hospitals take individual paths to going green
Hospitals across the country continue to chart new green territory by embracing tried-and-true sustainability methods and launching new initiatives that often are tailored to suit their individual budgets and staffing requirements.
Following is a sampling of health system initiatives underway, based on responses to the Health Facilities Management/American Society for Healthcare Engineering/Association for the Healthcare Environment 2015 Sustainable Operations Survey.
Energy management
Energy was the largest category in which respondents reported that they track and report savings from sustainable efforts, including these projects:
- One facility is realizing energy savings by installing variable-frequency drive chillers, changing to light-emitting diode lighting, reducing kitchen hood runtime, changing out older air handling units over the past five to seven years, and capitalizing a water side economizer for fiscal 2016. The result: The hospital’s Energy Star score of 10 in 2008 jumped to 41 in 2015.
- By converting from 32- to 25-watt lighting with start ballast and occupancy sensor switches, one facility has realized an annual savings of more than $150,000.
- A facility that installed solar electric panels on a warehouse building offset electric use at that building by more than 95 percent. Phase 2 of the facility’s Renewable Energy Program involves installing car canopies that will be covered with solar electric panels.
- Installing an absorption chiller with two 240-kilowatt turbines that run off the facility’s woodchip boiler means no oil or gas is burned.
- By connecting a chilled water system to a process condenser water system during a winter change-out of cooling towers, one facility realized a 27 to 50 percent reduction in steam consumption at the preheats.
- A facility retrocommissioned a medical clinic, resulting in a 60 percent reduction in energy usage and $55,000 annual savings with slightly more than a one-year payback.
- By replacing aged and worn-out steam boilers with floating head boilers, one orthopedic hospital cut natural gas use by 11 percent.
Waste management
Implementing a regulated medical waste program is the top waste management initiative being taken at health facilities, including these examples:
- With the help of nursing leadership, one facility trained nursing staff about proper waste stream disposal, and removed all biohazardous waste containers from patient rooms. (California law now allows nursing staff to hand-carry biohazardous waste bags without a secondary container.) The forecasted cost reduction is 20 to 24 percent the first year, possibly increasing to 35 percent.
- Implementing an integrated waste stream system through a vendor is saving one hospital 10 percent across the board or $28,000 annually.
- One facility is seeing a small cost reduction by switching to a vendor that allows for comingling of pharmaceuticals and sharps in the same container. This program validates a method pioneered by the facility’s caregivers.
Water conservation
Reducing water usage is a big focus at health facilities as costs continue to rise, as demonstrated by these initiatives:
- At one facility, water from three water-cooled compressors is captured and pumped into the cooling towers, reducing the amount of water at the towers, for an approximate savings of 36,000 gallons of water a year.
- Along with installing dual-flush handles during a retrofit and a laminar-flow retrofit, one hospital now requires all new projects to have low-flow fixtures and occupancy sensors, giving it an estimated water reduction of 3 million gallons.
- One facility launched an irrigation initiative after realizing they were using twice the water per acre as two other nearby facilities. By fixing leaks and installing weather-based controllers, the facility reduced irrigation water use by 1.5 million gallons in the three-month irrigation season alone.
Green cleaning
Cleaning materials to reduce water usage and eliminate chemicals also are being adopted by hospitals, including these examples:
- Along with switching from large mops to microfiber cloths and mops, one facility is changing to a hand soap without fragrance or color.
- One facility is stripping floors using only water via a machine that “sands” the surface rather than using harsh chemicals to remove old wax and finish. All new flooring that is installed has a no-wax finish.
- One facility is eliminating all aerosol products.
- Another facility is implementing a microfiber system to reduce water and chemical use.
Join Practice Greenhealth
Practice Greenhealth is the health care sector’s go-to source for information, tools, data, resources, and expert technical support on sustainability initiatives that help hospitals and health systems meet their health, financial, and community goals.
